Physical Therapy for Spinal Stenosis
Spinal stenosis is a degenerative condition of the spine that involves narrowing of the openings within the vertebrae of the spinal column that results in too much pressure on the spinal cord and nerves, causing pain and weakness in the low back. Spinal stenosis can develop after the age of 50 due to the effect of aging and osteoarthritic wear and tear on the spine and spinal vertebrae. Physical therapy provides an effective treatment for spinal stenosis, helping patients regain function, mobility, and strength in their low back and relieving compression of the spinal nerves.
Anatomy of the Lumbar Spine
The spine is comprised of a column of 24 vertebrae as well as the fused bones of the sacrum and coccyx bones that begin at the base of the skull and end at the pelvis. The spinal column protects the spinal cord and supports the body’s weight.
The spinal cord is made up of bundles of nerves that run through the tunnel formed by the vertebrae. The spinal cord sends and receives messages between the body and the brain and is surrounded and protected by the bony vertebrae of the spine. Nerve roots are the initial segment of a bundle of nerve fibers that exit the spinal cord through side spaces between the vertebrae called the neural foramen. The nerves then go out to all parts of the body.
Each vertebra consists of several parts: the body, which is the round front portion, a central ring-shaped opening (the spinal canal), flat bony areas (the facet joints) where one vertebra comes in contact with the vertebrae above and below it, and bony sections along the sides and back of the vertebral body. Between each vertebra is a flat, round pad called an intervertebral disk that serves as a cushion or shock absorber. The vertebrae are surrounded by ligaments, strong fiber bands that hold the vertebrae together, keep the spine stable, and protect the disks.
The lumbar spine is made up of five vertebrae in the lower part of the spine, between the ribs and the pelvis. The lumbar spine supports and stabilizes the upper body, allows movement of the trunk, protects the spinal cord, and controls leg movements.
What is Lumbar Spinal Stenosis?
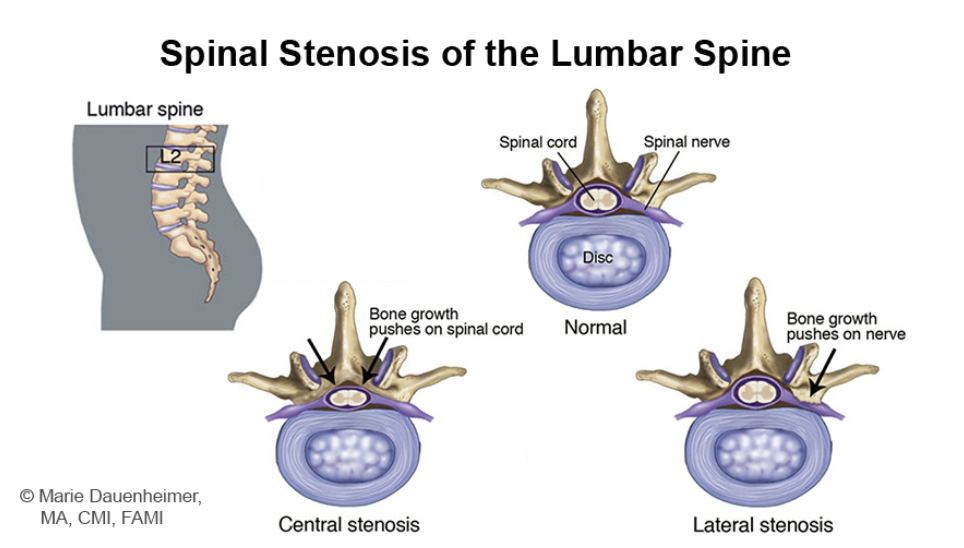
Spinal stenosis is a degenerative condition of the spine that involves narrowing of the openings within the vertebrae of the spinal column that results in too much pressure on the spinal cord and nerves. It most commonly occurs in the neck or the low back (the lumbar region of the back). Less space within the spine reduces the amount of space available for the spinal cord and the nerves that branch off the spinal cord, which can irritate, compress, or pinch the nerves and lead to significant pain.
When spinal stenosis occurs in the lumbar spine, a narrowing of the spinal cord occurs in the low back, placing pressure on the nerves extending from the lumbar vertebrae which can affect the function of the low back and legs. Spinal stenosis generally develops after the age of 50; women have a higher risk of developing it than men.
Symptoms of spinal stenosis can include:
Pain in the low back, either a dull ache or electric burning sensation
Heavy feeling in the legs, leading to cramping in one or both legs
Sciatica, pain originating from the low back extending through the buttocks and down the leg
Numbness or tingling in the legs, foot, or buttocks
Weakness in the leg or foot that worsens
Pain that increases when standing for a long time, walking downhill, or flexing backward
Pain that improves when you lean or bend slightly forward or walk uphill
In severe cases, loss of bladder or bowel control
Common causes of spinal stenosis include:
Osteoarthritis (OA): osteoarthritis, which involves a breakdown of the cartilage in joints causing the bones to rub against each other, can lead to bone growth and arthritic spurs. These bone spurs on the vertebrae can extend into the spinal canal and narrow the space, pinching nerves of the spine.
A bulging disk or herniated disk: As we age, the intervertebral disks between each vertebra can dry out, flatten, and crack, which can cause the gel-like center of these disks to break through and press on the nerves near the disk.
Thickened ligaments: ligaments are fiber bands that hold the spine together. However, arthritis can cause ligaments to thicken over time and bulge into the spinal canal space.
Spinal fracture or injury: A broken or dislocated bone and the subsequent inflammation near the spine can narrow the canal space and put pressure on spinal nerves.
Past spinal surgery: surgery can alter the structure of the spine or cause you to develop scar tissue in the spinal area, which can contribute to narrowing of the spinal canal or place pressure on spinal nerves.
Spinal cord cyst or tumor: a growth within the spinal cord or between the vertebrae and spinal cord can narrow the spinal cord space and place pressure on the spinal cord and nerves.
Congenital spinal issues: having a small spinal canal or having scoliosis (an abnormally shaped spine) can predispose you to developing spinal stenosis.
Physical Therapy for Spinal Stenosis
Physical therapy is the first line of treatment for spinal stenosis. The aim of the physical therapist during treatment is to improve the range of motion of the lumbar spine, reduce tightness in surrounding muscles, decrease pain and joint stiffness, relieve compression of nerves, strengthen the core and trunk muscles, improve postural alignment of the lumbar spine, and improve leg strength to help with overall balance and function.
A 2018 study found that physical therapy works just as well as surgery with fewer unwanted complications for the treatment of lumbar spinal stenosis. In the University of Pittsburgh study, 169 participants with lumbar spinal stenosis were divided into two groups: one group who had surgery right away and another group who did a specifically designed physical therapy program prior to considering surgery. Both groups saw benefits as early as 10 weeks post-surgery or after beginning physical therapy. Both groups experienced a decline in low back pain over a four-month period and their physical function continued to improve. When evaluated 2 years later, there was no difference in pain or physical function between the surgery and physical therapy groups. This indicates that physical therapy is just as effective in managing spinal stenosis as surgery. Researchers, therefore, recommend that those with lumbar spinal stenosis try a physical therapy program first to manage the condition prior to contemplating surgery.
Physical therapy treatment for spinal stenosis includes:
Pain management with ice and heat: ice helps to reduce swelling, tenderness, and inflammation to minimize pain, while heat therapy increases blood flow to the area, relaxes muscles, and relieves aching joints.
Gentle stretching of the low back muscles: stretching of both the muscles that run vertically along the spine as well as those running diagonally from the pelvis to the lumbar spine to relieve muscle tightness and pain and improve overall mobility and range of motion of the lumbar spine and vertebrae.
Stretching of the muscles of the hip: stretching of the hip flexors in the front of the hip, the piriformis in the back of the hip, and the hamstrings as these muscles attach to the pelvis, which directly connects to the lumbar spine. Restrictions in the hip muscles can directly affect the mobility of the lumbar spine.
Core strengthening: strengthening the abdominal muscles and the muscles of the trunk, pelvis, lower back, and hips help stabilize the lumbar spine and protect it from excessive movement and compressive forces.
Gluteal and leg strengthening to take the workload off the spinal joints.
Aerobic conditioning to increase tolerance for walking and daily activities.
Manual therapy: soft tissue and joint mobilizations to improve the mobility of stiff spinal joints.
Aquatic therapy: exercising in water helps to relieve the pressure exerted on the spine and allows the patient, due to the buoyancy of the water, to move with greater ease and less pain. The movement in water helps to increase blood flow to the surrounding muscles and joints to improve flexibility and muscle activation.
Posture education: posture training to minimize stress on the spine through proper alignment of the body.
Have you been diagnosed with lumbar spinal stenosis and are experiencing persistent pain? Work with a physical therapist today to manage pain and regain function and mobility in your low back!